Blood Component Transfusions
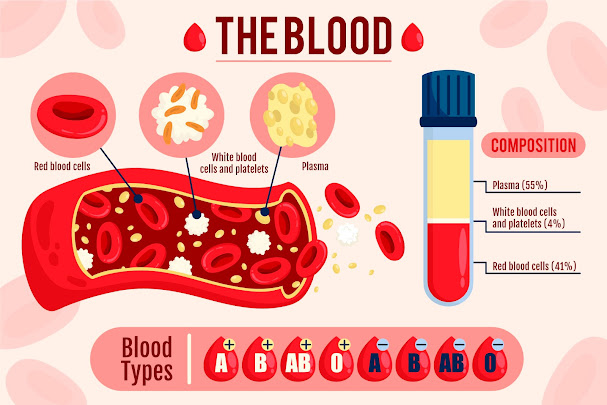
Blood component transfusions are one of the most commonly performed medical procedures. Tens of millions of transfusions take place during the span of a year within the United States. Transfusions can be required for many situations such as acute blood loss anemia due to trauma or surgery, blood cancers like leukemia, chemotherapy involved in treating leukemias, iron deficiency causing anemia, infections, etc. The vast majority of blood component transfusions are acquired through the selflessness and generosity of the general public donating their time and literally part of themselves to help save another life. In rare cases, a patient may elect to do an "autologous" donation in which they donate their own blood which can then be used for an upcoming surgery if the patient for any reason refuses an allogeneic (meaning not from one's self, but from someone else) transfusion.Donors must be screened ahead of time prior to donation to ensure they are healthy enough to donate and meet the requirements of a donor. Different donation types will typically have slightly different requirements. The vast majority of donations performed in the United States involves donating "Whole Blood" which will drain via gravity into a (usually) 500 milliliter(mL) donation bag. Whole Blood simply means that it contains the entirety of the circulating blood which is made up of Red Blood Cells (roughly 40-45% of the blood's composition), plasma (the straw yellow liquid portion of the blood comprising 50%+ of the total blood volume), and platelets/white blood cells.
The old catchphrase "You can save up to 3 lives with just one donation!" comes from the fact that the donated blood will then be sent to the Blood Center's manufacturing department. The blood will then be centrifuged (spun in a machine that goes several thousand rotations per minute) which causes the parts of the blood to separate. The blood center can then create individual products out of the layers. Packed Red Blood cells, Plasma (which is then frozen until use, and Platelets. Three separate products that can then be given to three separate lives in need. The white blood cells are almost universally always filtered out. The reason for this will follow on a separate page. There are only very specific instances in which White Blood Cells are wanted and used in transfusion.
 |
| Designed by pikisuperstar / Freepik |
All donations in the US must be screened for infectious diseases before it can be released to a transfusion center for use. The Blood Donation center will also perform a Blood Type on the donor unit. Every donation will be screened via laboratory testing for HIV (Human Immunodeficiency Virus) Types 1 and 2, Hepatitis B, Hepatitis C, HTLV (Human T-Lymphotropic virus) I and II, Treponema pallidum (the causative agent of Syphilis), West Nile Virus, and Zika virus. All first time donors will be tested for Trypanosoma cruzi the causative agent of Chagas disease. All platelets will be screened for bacterial infection via culture every donation as well. Other infections that may be screened for include Babesia and Cytomegalovirus.
 |
| Donor Blood draining through a leukoreduction filter |
Directed donation is another form of donation in which a close family member or friend donates blood products for the patient in need. This is more common than a Paid Donor situation, but also happens very infrequently, at least in the United States. Similar problems can occur involving friends or family members lying about their medical history potentially jeopardizing the health of the recipient. Donations from close relatives can also pose other risks such as transfusion related Graft vs Host disease in which the white blood cells remaining after leukoreduction can start to activate and attack the cells of the recipient. More about this in the transfusion reaction section.
Once infectious disease testing is completed, the components have been fully manufactured, the units have been labeled appropriately, and the blood is determined to be safe for transfusion the Blood Center can officially send it out to transfusion centers. The most common recipient of blood products are hospital Blood Banks. Blood Banks are overseen medically usually by a Pathologist specializing in Transfusion Medicine. Pathologists are medical doctors. The employees of a hospital Blood Bank consist mostly of Medical Laboratory Technicians and Medical Laboratory Scientists (a 2 and 4 year degree, respectively). Some may have their masters, and some may have a Blood Bank specialist certification. These specialist employees may be in managerial/supervisory roles, or work in a Lead Technologist role on their shift. Other Blood Bank members such as lab assistants, generally only need a High School or High School equivalent.
Transfusions are a very safe procedure with heavy regulation and guidelines backing it to ensure the process goes smoothly from donation to transfusion.